
Congenital Diaphragmatic Hernia
Congenital Diaphragmatic Hernia
Congenital Diaphragmatic Hernia (CDH) is a developmental defect of the diaphragm that allows the abdominal contents to herniate into the chest. It occurs in approximately 1/2500 live births. Most defects are left sided (80-85%). CDH is commonly classified into 3 categories based on location.
Pathophysiology
Herniation of the abdominal contents results in ongoing poor growth of the lung on the same side and also secondary mass effect leading to subsequent poor growth on the opposite side lung too. These changes lead to t:
- Lung mechanics: reduced lung volumes.
- Pulmonary vasculature: Decreased blood vessel branches that leads to reduced cross-sectional area of the capillary bed and increased thickness of the small vessels leading to difficulty in absorption of oxygen by blood.
- The lungs will be more resistant to treatment with mechanisms such as nitric oxide therapy.
Clinical Presentation
- Most infants with CDH will be diagnosed antenatally. Right sided CDH may be missed as the liver and lung may be difficult to differentiate on scan. Commonly bowel loops along with or without liver herniate. Polyhydramnios (excess amniotic fluid) is common. Cardiac anomalies are difficult to diagnose due to abnormal position and rotation of the heart.
Antenatal:
Postnatal
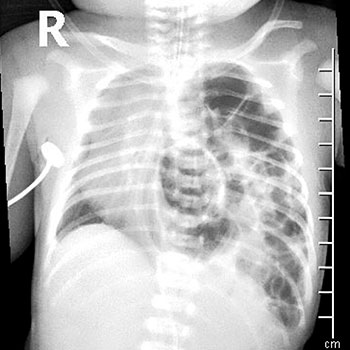
- Classically, a newborn presents with severe respiratory distress (breathlessness), barrel – shaped chest, empty appearing (incurved) abdomen. On clinical exam, theabreath sounds are reduced on the side of the CDH and the heart sounds best heard on the opposite side of the chest.
- Positioning should be semi upright to reduce nasal regurgitation and reflux.
- About 5% of CDH will present at > 24 hours of age with mild fast breathing, or later still with poor growth, recurrent pneumonias or as an chance finding on a chest x-ray done for another reason.
Investigations
- Chest x-ray
- Ultrasound or chest CT, if chest x-ray is able to confirm the diagnosis.
- Echocardiography to exclude congenital heart disease.
- Genetic testing: Karyotype and/or micro-array.
- Renal and head ultrasound to exclude any other associated anomalies.
Management at birth
- All antenatally diagnosed CDH infants require endotracheal intubation (breathing tube) at birth electively.
- Cardiac and oxygen saturation monitoring.
- Insert a feeding tube / nasogastric tube.
- Shift to NICU for ventilator and further management.
Surgical Considerations
- Surgery is delayed to allow for haemodynamic stability, reduction in lung blood pressure (pulmonary hypertension), appropriate ventilation and correction of any other disturbances.
- A daily discussion with the paediatric surgeon regarding the timing of surgery is required.
- In unfortunately circumstances, where the baby has not responded and continued to deteriorate despite maximal therapies being instituted, a palliative care approach should be considered in discussion with the family.
Discharge Planning and Follow-up
- Infants who have had a CDH repair require a prolonged time on the ventilator / NICU.
- These infants should go into neonatal developmental follow-up programme (4, 8, 12, 18, 24 months) to monitor growth and identify other developmental problems early and resolved.