
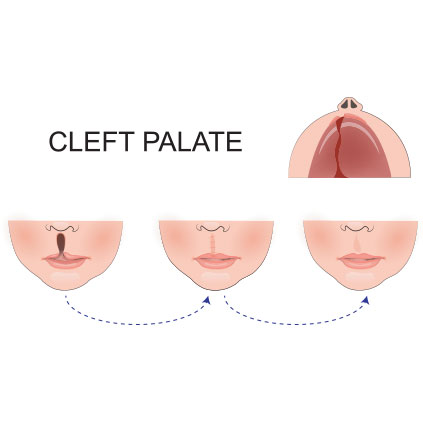
Cleft Lip and Cleft Palate
Cleft Lip and Cleft Palate
Cleft lip and/or palate malformation is caused by a failure of the normal oro-facial development between 6 and 12 weeks of intrauterine life. The incidence is 1:1000 Caucasian births and higher in Asian populations. It is more common in males and can be associated with other abnormal structures.
All infants born with a cleft lip and/or palate should be assessed immediately after birth by the paediatric team. This assessment determines if there are any airway concerns, and if so, what is the appropriate form of monitoring, where the baby should be monitored and if there are any other associated anomalies. At this review a feeding plan also needs to be formulated with parents. In mild cases, baby needs admission to NICU for 3 – 4 days for establishment of feeds, parent education and resolution of breathing difficulties.
During admission, the child is also assessed by the plastic surgical team to discuss the timing of definitive surgery for the lip and palate. Repair of the lip occurs at approximately 3 - 6 months and repair of the palate at 6 - 9 months.
Feeding
- Infants with cleft lip and or palate are routinely fed with a squeezy bottle with a short, fast teat as they are generally unable to create an adequate seal to feed or if breast feeding, introducing extra breast into the mouth of the baby so that the breast is pushed against the hard palate and forms the upper wall whilst breast feeding.
- Infants should be fed in a sitting up position to prevent the risk of aspiration. If a baby is fed in the more usual cradled position, milk may pool in the oral cavity and aspiration may occur.
- As infants with clefts do not maintain a good seal, they tend to swallow a lot of air with the feed and therefore require burping at the middle and end of the feed.
- Breast feeding, although difficult, may be possible for infants with minor clefts, especially after a good milk supply has been established. Mothers should be encouraged to express breast milk. Expressed milk can be given via a bottle.
Recommendations to Assist with Breastfeeding Support
- Mothers should be encouraged to provide the protective benefits of breast milk, in preference to formula milk.
- Monitoring of hydration and weight gain is important, if inadequate, supplementary feeds should be implemented or increased. These should ideally be expressed breast milk and given via a bottle.
- A small or preterm baby with a cleft will have less reserves so may also have more difficulty breastfeeding.
- Consideration should be given to allowing smaller volumes of expressed breast milk for healthy term babies in the first 48 hours as this is what they would be receiving if normally breastfeed. This should be monitored closely by weight and assessment of hydration during this period. Modification of breastfeeding positions may increase the efficiency and effectiveness of feeding. Skin to skin can provide comfort for the infant and aid lactation especially when breastfeeding is difficult.
Positioning the Infant for Breastfeeds
- Infants with CL should be held so the CL is orientated towards the top of the breast. The mother may occlude the CL with her thumb or finger and/or support the infant’s cheeks to decrease the width of the cleft and increase closure around the nipple.
- Positioning should be semi upright to reduce nasal regurgitation and reflux.
- Mothers may need to manually express breast milk into the baby’s mouth to compensate for absent suction, and compression and to stimulate the let down reflex.
Prior to Discharge
- Parents must be competent in feeding and mouth care. The infant should be feeding well and gaining weight.